Introduction
Benzodiazepines, often prescribed to alleviate anxiety, insomnia, and seizures, are classified as Schedule IV controlled substances. Common examples include Xanax, Valium, and Ativan. While effective for short-term use, prolonged benzodiazepine use can lead to physical dependence, making cessation challenging and potentially causing significant withdrawal symptoms. A carefully planned Benzo Taper Schedule is crucial for minimizing these risks and ensuring a safer withdrawal process. This article, based on expert insights and patient experiences, aims to provide a comprehensive guide to understanding and creating an effective benzo taper schedule. It is vital to understand that physical dependence is distinct from addiction, and misinterpreting dependence as addiction can lead to harmful rapid withdrawal approaches.
Benzodiazepine Dependence vs. Addiction: Key Differences
It’s essential to differentiate between physical dependence and addiction. Physical dependence is a normal physiological adaptation to chronic medication use, where the body adjusts to the drug’s presence. Withdrawal symptoms occur when the medication is reduced or stopped. Addiction, on the other hand, is a complex behavioral disorder characterized by compulsive drug seeking and use despite harmful consequences. The FDA and DSM-V emphasize that physical dependence is not addiction and is an expected response to many prescribed medications affecting the central nervous system. Mistaking dependence for addiction can lead to dangerously rapid or forced cessation, causing significant harm.
How Benzodiazepines Change Your Body and Necessitate a Taper Schedule
Benzodiazepines enhance the effects of GABA, a neurotransmitter that calms brain activity. Long-term use can lead to changes in GABA receptor sensitivity. One theory suggests that chronic benzodiazepine exposure may downregulate GABA receptors, while withdrawal and cessation may eventually upregulate them. GABA receptors are distributed throughout the body and play a crucial role in the central nervous system and stress response. These adaptations underscore the importance of a gradual benzo taper schedule to allow the brain and body to readjust slowly, minimizing withdrawal severity.
Common Misguided Cessation Methods and Why a Structured Benzo Taper Schedule is Essential
Overly Rapid Tapers: The Pitfalls of Speed
A common but often problematic method is reducing the benzodiazepine dose by 25% weekly. While seemingly gradual to some prescribers, this approach is often too rapid, failing to allow the body sufficient time to adapt. Research indicates that such rapid tapers are ineffective for a significant percentage of long-term users, with many experiencing withdrawal symptoms and failing to achieve complete cessation. Rapid tapering increases the risk of protracted withdrawal syndrome (PAWS), which can cause debilitating symptoms lasting months or even years. In severe cases, overly rapid withdrawal can even lead to seizures and life-threatening complications.
Skipping Doses: Inconsistent Drug Levels and Increased Suffering
Another flawed method involves skipping doses throughout the week. This approach creates fluctuations in drug serum levels, leading to peaks and valleys that can trigger withdrawal symptoms. Instead of a steady decline, skipping doses can cause unnecessary suffering and instability, making a consistent benzo taper schedule significantly more effective. Patients highly sensitive to benzodiazepines can experience severe reactions even to minor dosage variations. Attempting to split pills for smaller dose adjustments is often inaccurate and can further exacerbate symptom fluctuations, highlighting the need for more precise tapering methods.
Effective Benzo Taper Schedule Styles: Dry vs. Liquid, Cut & Hold vs. Micro-Taper
Safe benzodiazepine cessation can be achieved through various tapering styles, categorized by delivery method (dry or liquid) and reduction style (cut and hold or micro-taper). Most benzodiazepines are not manufactured in dosages conducive to easy tapering, necessitating dose manipulation through cutting, compounding, or liquid solutions.
Cut and Hold Benzo Taper Schedule: Gradual Dose Reduction
The “cut and hold” method involves reducing the current dose by a small percentage (typically 5% to 10%) and maintaining this dose until withdrawal symptoms stabilize. This stabilization period can take several weeks, allowing the nervous system to adjust before further reductions. This is a straightforward approach to creating a benzo taper schedule that prioritizes comfort and gradual adaptation.
Micro-Taper Benzo Taper Schedule: Minimizing Withdrawal Fluctuations
Micro-tapering, developed within online support communities, involves very small, daily dose reductions, typically totaling no more than a 5% to 10% reduction from the current dose each month. These daily micro-reductions aim to minimize the fluctuations in drug levels and the associated withdrawal symptoms that can occur with larger, less frequent reductions. A micro-taper benzo taper schedule often requires detailed tracking using a log or spreadsheet to manage the daily adjustments.
Dry Taper Methods: Practical Approaches
Dry tapering is a popular method due to its convenience. It involves physically manipulating tablets using pill cutters or scales to reduce the dose. Dry tapering can be implemented using both cut-and-hold and micro-taper techniques. The Ashton Manual, a highly respected guide in the benzodiazepine withdrawal community, also utilizes a dry taper approach with diazepam.
The Ashton Manual Benzo Taper Schedule: A Diazepam-Focused Approach
The Ashton Manual, developed by the late Dr. Heather Ashton, is a widely recognized and respected guide for benzodiazepine withdrawal. Dr. Ashton’s clinic reported a 90% success rate using her protocol, which emphasizes switching to diazepam for tapering due to its long half-life and availability in lower doses. Diazepam’s long half-life helps prevent interdose withdrawal symptoms. Compared to shorter-acting benzodiazepines like clonazepam and alprazolam, diazepam’s dose flexibility makes it more suitable for gradual reduction.
While the Ashton Manual initially recommended diazepam substitution, newer guidelines suggest staying on the original benzodiazepine if withdrawal symptoms are manageable. Switching to diazepam carries risks of adverse reactions to the new medication, and some find the Ashton Manual’s taper rate too fast. Additionally, the switch to diazepam can add time to the overall taper process. It’s crucial to individualize the benzo taper schedule based on patient response rather than strictly adhering to a pre-set rate.
Tapering Strips: Pre-Packaged Gradual Dose Reductions
Tapering Strips, developed by Dr. Peter Groot in the Netherlands, offer pre-packaged, gradual dose reductions, adjustable to individual needs. These strips are available for several benzodiazepines, including Ativan, Valium, and Klonopin. While Tapering Strips offer a convenient, structured benzo taper schedule, their availability may be limited by geographical location due to international shipping restrictions and regulations.
Dry Micro-Taper with a Scale: Precise Dose Measurement
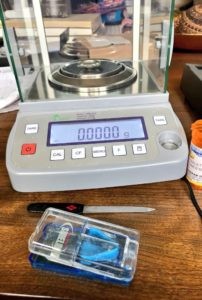
For those requiring highly precise dose reductions, dry micro-tapering with a scale allows for daily reductions as small as 0.001 to 0.003 grams. While initially daunting, this method offers fine-grained control over the benzo taper schedule. Online resources and support groups provide guidance on implementing this technique, which is particularly useful when liquid methods are not feasible.
Liquid Taper Methods: Enhanced Dose Control
Liquid tapering offers greater control over dose reduction, allowing for smaller, more frequent adjustments. It also facilitates multiple daily dosing, which can help stabilize drug levels and minimize interdose withdrawal symptoms. Liquid methods are particularly suited for implementing micro-taper benzo taper schedules.
Manufacturer’s Oral Solution: Convenient Liquid Dosage
When available, manufacturer’s oral solutions provide a straightforward liquid tapering option. For example, diazepam oral solution allows for reductions as small as 0.05 mg using a 1 mL syringe. For even smaller increments, the solution can be further diluted with water, offering a highly customizable benzo taper schedule.
Compounding Pharmacies: Customized Liquid Formulations
Compounding pharmacies can prepare customized liquid solutions from prescription benzodiazepines, using suspending agents to create stable formulations. Liquid compounds offer ease of dose control and can reduce the workload associated with dry tapering methods, although they may be more expensive and not always covered by insurance. Choosing a pharmacy associated with professional compounding organizations ensures quality and expertise.
Water/Milk Titration Method: A DIY Liquid Approach
The water or milk titration method is a layperson-developed liquid tapering technique. It involves dissolving or suspending a benzodiazepine pill in a measured amount of liquid and then discarding a portion of the suspension to reduce the dose. While accessible, this method has limitations as most benzodiazepines are not fully water-soluble, requiring thorough shaking to ensure dose consistency. Despite its imperfections, water titration provides a DIY liquid benzo taper schedule for those who cannot tolerate compounded liquids.
Key Tapering Strategies for a Successful Benzo Taper Schedule
Recommended Taper Rate: Slow and Steady Wins
A general guideline for a safe benzo taper schedule is to reduce the current dose by no more than 5% to 10% every four weeks. This slow rate contrasts sharply with rapid reduction methods and is supported by research indicating the ineffectiveness of faster tapers. Individual responses vary, and the taper rate should be adjusted based on symptom tolerance.
Benzodiazepine Conversion Rates: Switching Medications
Switching from a shorter-acting to a longer-acting benzodiazepine, like diazepam, can be part of a benzo taper schedule. Conversion charts, such as those developed by Dr. Ashton, provide estimated equivalent doses. However, these are guidelines, and individual responses can vary. It’s crucial to allow patients to determine their optimal conversion dose, adjusting as needed based on withdrawal symptoms. Benzodiazepine equivalency is not strictly regulated, emphasizing the need for patient-centered adjustments.
Multiple Daily Dosing: Maintaining Stable Drug Levels
For many, dividing the daily benzodiazepine dose into multiple smaller doses throughout the day can significantly improve tolerability. This strategy helps maintain more stable drug serum levels, reducing peaks and valleys that can trigger withdrawal symptoms. The frequency of dosing depends on the benzodiazepine’s half-life, with shorter-acting medications often requiring more frequent dosing. A well-structured benzo taper schedule should consider dose frequency to optimize patient comfort.
Medications to Alleviate Withdrawal Symptoms: Proceed with Caution
Currently, no FDA-approved medications specifically target benzodiazepine withdrawal symptoms. While some medications like gabapentin, clonidine, and antidepressants are sometimes suggested, their effectiveness is not well-established, and they may introduce new side effects or require their own tapers. Expert guidelines, like the British National Formulary, advise against the routine use of add-on medications in benzodiazepine withdrawal. Patient reports suggest increased sensitivities to other medications during benzodiazepine withdrawal, highlighting the importance of minimizing unnecessary drug exposure during a benzo taper schedule.
Conclusion: Prioritizing Patient Safety in Your Benzo Taper Schedule
Patient safety is paramount in benzodiazepine cessation. While no method guarantees a completely symptom-free withdrawal, the strategies outlined in this guide, focusing on slow, patient-centered benzo taper schedules, can significantly improve the chances of successful and tolerable withdrawal. Rapid withdrawal is generally riskier once physical dependence has developed, and should only be considered in very rare circumstances, such as paradoxical reactions to the drug. Whether working with a healthcare provider or self-managing, a comfortable, patient-directed taper is essential. Forced or overly rapid tapers should always be avoided, and patients should be empowered to choose a benzo taper schedule that respects their individual needs and responses, maximizing their opportunity for successful cessation and long-term well-being.