Benzodiazepines, commonly known as anxiolytics, are classified as Schedule IV controlled substances and are frequently prescribed to manage anxiety, insomnia, seizures, and alcohol withdrawal. However, their use extends to numerous off-label applications including restless leg syndrome, muscle spasms, tinnitus, dementia, mania, and akathisia. Common examples of benzodiazepines include Klonopin (clonazepam), Ativan (lorazepam), Xanax (alprazolam), Valium (diazepam), Onfi (clobazam), Tranxene (clorazepate dipotassium), and Librium (chlordiazepoxide).
Medical guidelines generally advise against continuous benzodiazepine use beyond two to four weeks. Despite varying estimates, a significant portion of individuals using benzodiazepines long-term (exceeding two to four weeks) develop physical dependence and encounter difficulties when attempting to discontinue these medications safely. Regardless of their desire to stop, many individuals experience severe mental and physical withdrawal symptoms.
Predicting who will experience complicated withdrawal from benzodiazepines is impossible at the outset of treatment or cessation. For some, stopping benzodiazepines can become a protracted and life-altering process due to complex withdrawal syndromes. Therefore, both healthcare providers and patients must be well-informed about effective tapering strategies. The methods detailed below are based on clinical experience, research, and insights from patients who have successfully navigated benzodiazepine tapers.
Understanding Physical Dependence vs. Addiction in Benzo Tapering
It’s crucial to differentiate between prescribed physical dependence and addiction. Misinterpreting physical dependence as addiction has led to harmful practices, such as forced or overly rapid cessation, causing significant patient harm. Further clarification is available from the:
FDA guidance which helps distinguish between physical dependence, addiction, and abuse, stating clearly:
Physical dependence is not synonymous with addiction; a patient may be physically dependent on a drug without having an addiction to the drug. Similarly, abuse is not synonymous with addiction. Tolerance, physical dependence, and withdrawal are all expected biological phenomena that are the consequences of chronic treatment with certain drugs. These phenomena by themselves do not indicate a state of addiction.
Similarly, the DSM-V (Diagnostic and Statistical Manual of Mental Disorders) emphasizes:
“Dependence” has been easily confused with the term “addiction” when, in fact, the tolerance and withdrawal that previously defined dependence are actually very normal responses to prescribed medications that affect the central nervous system and do not necessarily indicate the presence of an addiction.
How Benzodiazepines Change the Body During Long-Term Use
The exact physiological mechanisms behind benzodiazepine tolerance and withdrawal remain unclear. One prevalent theory suggests that long-term benzodiazepine use, which enhances the neurotransmitter GABA (gamma-aminobutyric acid) at GABA-A receptors, may lead to a downregulation of these receptors. Conversely, discontinuation may eventually upregulate them. GABA receptors are distributed throughout the body and play vital roles in the central nervous system and stress response.
Common Cessation Methods and Their Pitfalls
The Problem with “Slow” Tapers That Are Too Fast
A frequently used, yet often inappropriate, method involves reducing the benzodiazepine dose by one-quarter each week. This approach aims to complete tapering within a few weeks. While some prescribers might consider this gradual, experts, researchers, experienced clinicians, patients, and prescribing guidelines often deem such tapers too rapid. A four-week taper often does not allow sufficient time for the body to adapt. Research indicates that this rapid tapering method is ineffective for 32% to 42% of long-term benzodiazepine users in achieving a drug-free state, with approximately 90% experiencing withdrawal symptoms.
Many patients subjected to such rapid tapers have developed protracted withdrawal syndrome (PAWS). This condition can persist from eighteen to twenty-four months, or even years in some cases. A slower, more gradual dose reduction can mitigate the severity of withdrawal and the risk of PAWS. Furthermore, rapid tapers increase the risk of seizures and, in severe cases, death.
Image depicting pills and a hand, illustrating the process of benzo tapering. Alt text: Pictured are pills and a hand, representing the careful dose reduction necessary during a benzo taper.
Individuals with physical dependence can become highly sensitive to benzodiazepines, where even slight dose variations can cause significant distress. Pill splitting, often attempted to achieve smaller dose reductions, is inherently inaccurate because pills are typically scored only in halves, if at all. Trying to split pills into quarters for even dose distribution is often ineffective and can worsen symptom severity and fluctuations during tapering.
The Drawbacks of Skipping Doses
Another common, yet problematic, tapering method involves reducing one daily dose per week over several weeks until all doses are eliminated. This approach shares similar disadvantages with the one-quarter weekly reduction method. Observations from online support groups, encompassing over a hundred thousand patients by the Benzodiazepine Information Coalition, reveal that this “reduce one daily dose a week” strategy frequently triggers debilitating mental and physical symptoms that can last for months or years. This may be due to the serum level fluctuations caused by skipped doses, leading to peaks and troughs in drug concentration. Such fluctuations can induce cycles of withdrawal, causing unnecessary suffering compared to a consistent, gradual dose reduction.
Benzo Tapering Methods: Finding the Right Approach
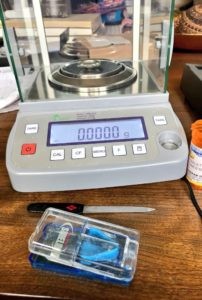
Safe benzodiazepine cessation can be achieved through dry (tablet-based) or liquid tapering methods, using either a “cut and hold” or “micro-taper” reduction style. While numerous effective approaches exist, the challenge is that most benzodiazepines are not available in dosages or formulations conducive to easy tapering. Therefore, dosage manipulation is almost always required, whether through pill cutting with a scale, compounding, or liquid solutions.
Cut and Hold Tapering
The “cut and hold” method involves reducing the current dose by a small percentage (typically 5% to 10% of the current dose) and maintaining this dose until withdrawal symptoms stabilize. It often takes several weeks for the nervous system to adjust after each reduction.
Micro-Tapering for Benzo Withdrawal
Online communities have developed “micro-tapering” techniques to ensure a more consistent and gradual dose reduction, aiming to minimize withdrawal symptoms. Micro-tapering involves daily, minute reductions, accumulating to no more than a 5% to 10% overall reduction from the current dose each month.
Daily micro-reductions can be particularly beneficial for individuals highly sensitive to dose changes, helping to avoid the physical and psychological distress associated with larger, weekly reductions. Tracking dose reductions during micro-tapering usually requires a daily log or spreadsheet.
Dry Benzo Tapering Methods Explained
Dry tapering is favored for its simplicity and convenience, often seeming more straightforward initially. It involves using pill cutters or scales to cut or shave off portions of a tablet for dose reductions. Dry tapering includes methods like “cut and hold” (periodic reductions of milligram amounts, perhaps monthly, holding until stabilization) and micro-tapering (frequent removal of very small, microgram amounts, possibly daily, adjusting based on symptoms).
The Ashton Manual: A Cornerstone of Benzo Tapering
The Ashton Manual, authored by the late psychopharmacologist Dr. Heather Ashton, is the most respected and well-known guide for benzodiazepine withdrawal within the patient community. Dr. Ashton’s clinic in the UK reported a 90% success rate over fourteen years using her protocol, which advocates for using diazepam for tapering. Diazepam’s long half-life (up to 200 hours) helps prevent interdose withdrawal symptoms. Additionally, diazepam is available in lower doses than newer, shorter-acting benzodiazepines, making it better suited for gradual dose reductions.
In contrast, clonazepam has a medium half-life and a minimum dose of 0.125 mg, while alprazolam has a short half-life and a minimum dose of 0.25 mg. These may seem like small doses, but their diazepam equivalency (0.125 mg clonazepam ≈ 2.5 mg diazepam; 0.25 mg alprazolam ≈ 5.0 mg diazepam) reveals they are not. Direct discontinuation from these doses is discouraged, necessitating reductions smaller than half or a quarter of the lowest manufactured dose—impossible to achieve accurately by simply breaking pills. (Further discussion in: Why Currently Available Benzodiazepine Doses Prevent Safe Withdrawal.)
Regarding tapering speed, the Ashton Manual suggests an average taper duration of ten months or longer, depending on the starting dose and individual patient response. Dr. Ashton emphasized patient-directed tapering pace based on physiological response to dose reductions. If symptoms become severe, pausing the taper for a few weeks until stabilization is advisable before resuming. Benzodiazepine tapers often take considerably longer than initially anticipated by both patients and prescribers.
While Dr. Ashton recommended diazepam due to its long half-life, more recent guidelines suggest staying with the originally prescribed benzodiazepine if withdrawal symptoms are manageable. Switching to diazepam introduces potential adverse reactions to a new medication. Moreover, some find the Ashton Manual’s suggested taper rate too fast and its reduction steps too large. Switching to diazepam can also prolong the overall process, adding weeks before tapering can even begin or resume, which can be discouraging. Finally, differentiating between adverse reactions to diazepam and general benzodiazepine withdrawal symptoms can be challenging.
Hear Dr. Ashton discuss her Manual:
Tapering Strips: A Modern Approach
Tapering Strips, developed by Dr. Peter Groot in the Netherlands, are a relatively new option for benzodiazepine tapering. These pre-prepared strips offer gradual, patient-adjusted dose reductions. Tapering Strips are available for Ativan (lorazepam), Valium (diazepam), Klonopin (clonazepam), Serax (oxazepam), Restoril (temazepam), and Imovane (zopiclon). Availability outside the Netherlands may be limited due to regulations, as they cannot ship substances on the Netherlands’ Opium Law list, which includes most benzodiazepines, internationally. However, within the Netherlands, they can be prescribed and ordered for delivery within about a week.
Listen to Dr. Groot explain Tapering Strips:
Dry Micro-Tapering with a Scale: Precision Dosing
Micro-tapering using a scale involves daily or every-few-days reductions, typically between 0.001 and 0.003 grams. This method can seem daunting initially, but resources and videos in online support groups explain various approaches. Patients finding the Ashton Manual’s reduction rate too rapid, but unable to use liquid methods, sometimes opt for this precise dry micro-tapering.
Liquid Benzo Tapering Methods for Gradual Reduction
Liquid tapering allows for finer dose adjustments, slower reduction rates, and more frequent dosing, which can minimize interdose withdrawal effects and facilitate daily micro-tapers.
Reductions in micro-tapers are cumulative, continuing until the dose is low enough for complete cessation. The reduction size (in milliliters or the milligram-to-milliliter ratio) can be easily adjusted to slow down the tapering rate if needed.
Manufacturer’s Oral Solutions for Benzo Tapering
Using a manufacturer’s oral solution, when available, allows for very small dose reductions and daily micro-tapering.
For instance, diazepam oral solution (e.g., Roxane Laboratories in the U.S.) is available at 5 mg / 5 mL (1 mg/mL). Using a 1 mL oral syringe, reductions as small as 0.05 mg to 0.10 mg can be made daily or every few days, depending on individual response, current dose, and desired reduction rate. For even smaller reductions, the manufacturer’s solution can be further diluted with water.
For patients intolerant to oral diazepam solution or diazepam itself, compounded liquid solutions of their original benzodiazepine can be prescribed.
Compounding Pharmacies: Customized Liquid Formulations
Compounding pharmacists can create oral solutions from prescriptions, combining suspending agents like OraPlus with crushed pills or benzodiazepine stock powder. (Pharmacists use databases to select appropriate suspending agents for each benzodiazepine.) Liquid compounds offer greater control over tapering rates and can be less labor-intensive, though they can be costly and may not be fully covered by insurance. It is recommended to choose pharmacists associated with the International Academy of Compounding Pharmacists or the Professional Association of Compounding Pharmacists.
Water/Milk Titration: A DIY Liquid Tapering Method
The “water titration” or “discard method,” a patient-developed liquid tapering technique, is used in online support communities. Some use it when compounded liquids are not tolerated, perhaps due to suspending agent sensitivities.
In water titration, a pill is crushed or dissolved in a measured amount of milk or water to create a suspension. Using an oral syringe, a portion of the suspension (measured in milliliters) is removed and discarded, while the remainder is ingested. Holds are recommended if symptoms become unbearable.
A drawback is that most medications are not fully water-soluble, requiring shaking the suspension to ensure even medication distribution.
Here’s a video explaining a water titration method:
Another video explains a milk titration method:
Key Benzo Tapering Strategies for Success
Recommended Benzo Taper Rate: Slow and Steady
A general guideline is to reduce the current dose by no more than 5% to 10% every four weeks. A study showed that a common physician-used “tapering” method—25% weekly reduction—failed for 32% to 42% of patients in achieving drug cessation.
Benzodiazepine Conversion Rates: Switching Medications
Image of a benzodiazepine conversion chart. Alt text: Benzodiazepine conversion chart illustrating equivalent doses of various benzodiazepines, helpful for switching medications during a benzo taper.
For switching from shorter-acting to longer-acting benzodiazepines for tapering, conversion calculations are crucial. Dr. Heather Ashton’s conversion guide proved effective in her clinic, though it can differ from other charts and physician opinions. Patient comfort should dictate conversion doses and reduction rates. If a conservative conversion leads to underdosing or withdrawal, increasing the dose to a comfortable level before reducing again is advisable. Unlike opioids, benzodiazepine equivalents are not FDA-mandated, and individual responses vary.
Multiple Daily Dosing for Benzo Tapering
Depending on a benzodiazepine’s half-life, multiple daily doses (maintaining the same total daily amount) can be beneficial. Evenly spaced doses can improve taper success by preventing serum level fluctuations that can make discontinuation intolerable.
For example, diazepam users might benefit from dividing doses into two or three daily intakes; clonazepam users, three or four; lorazepam users, four or five; and alprazolam users, five or six daily doses to maintain stable serum levels. Doses should be as evenly spaced as possible.
Medications to Manage Benzo Withdrawal Symptoms: Use with Caution
Currently, no FDA-approved medications specifically target benzodiazepine withdrawal symptoms. Add-on medications like Neurontin (gabapentin), Lyrica (pregabalin), Catapres (clonidine), BuSpar (buspirone), and various antidepressants are sometimes suggested, but are not necessary for tapering and may even be counterproductive. Evidence for their effectiveness in withdrawal is limited, and some may require their own lengthy tapers and introduce new side effects. The British National Formulary advises: “The addition of beta-blockers, antidepressants, and antipsychotics should be avoided where possible.”
Benzodiazepine Information Coalition observations from online support groups, representing over a hundred thousand patients, indicate that many withdrawing individuals develop heightened sensitivities to other medications, potentially exacerbating withdrawal symptoms.
Conclusion: Prioritizing Patient Safety in Benzo Tapering
Patient safety is paramount in benzodiazepine cessation. While no method guarantees a painless withdrawal, the discussed strategies can facilitate a more tolerable taper and maximize the chance of successful, complete healing.
In rare situations, rapid withdrawal might be considered if the drug causes a paradoxical response, though this is infrequent. While rapid withdrawal might seem desirable for those wanting to stop benzodiazepines quickly, it is often the riskiest and most dangerous approach once physical dependence has developed.
Whether working closely with a prescriber or withdrawing with limited support, patients should taper at their most comfortable pace. Forced tapers or abrupt cessation against a patient’s will should never occur. As outlined, numerous methods allow for benzodiazepine withdrawal without resorting to rapid tapers, excessively large reductions, or cold turkey approaches, ensuring a safer and more patient-centered process.