The dangers of mixing drugs can be severe, and combining certain substances can lead to life-threatening consequences. One particularly risky combination is opioids with benzodiazepines, often referred to as “Benzo Pills”. Co-use significantly elevates the risk of overdose, as highlighted by the U.S. Centers for Disease Control and Prevention (CDC).
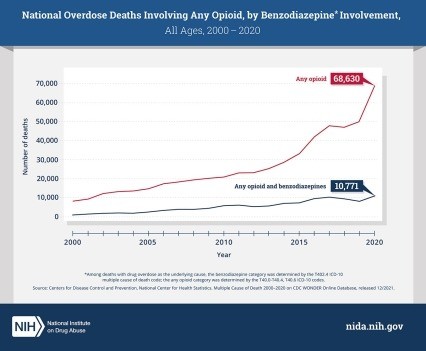 Line graph showing the increase in opioid overdose deaths in the United States from 2000 to 2020, highlighting the significant rise in deaths involving benzodiazepines, commonly known as benzo pills. Data from the National Institute on Drug Abuse (NIDA) indicates a substantial overlap between opioid and benzodiazepine-related overdose fatalities.
Line graph showing the increase in opioid overdose deaths in the United States from 2000 to 2020, highlighting the significant rise in deaths involving benzodiazepines, commonly known as benzo pills. Data from the National Institute on Drug Abuse (NIDA) indicates a substantial overlap between opioid and benzodiazepine-related overdose fatalities.
In fact, statistics from 2021 reveal a concerning trend: nearly 14% of all opioid overdose fatalities also involved benzodiazepines. Benzo pills, or benzodiazepines, are prescription sedatives frequently used to treat anxiety and insomnia. These medications, which include common names like Valium (diazepam), Xanax (alprazolam), and Klonopin (clonazepam), work by increasing the levels of GABA, a neurotransmitter that slows down brain activity, leading to a calming or sedative effect.
Adding to the complexity, benzodiazepines have been found in the illicit opioid supply in certain regions. This alarming discovery suggests that individuals might be unknowingly or knowingly consuming benzo pills alongside illicit opioids, further compounding the risks.
The Heightened Overdose Danger: Opioids and Benzo Pills
Every day, approximately 220 lives are lost in America due to opioid overdoses. The danger escalates dramatically when opioids are combined with benzo pills. Both drug types share a critical side effect: they can cause sedation and, crucially, suppress breathing. Respiratory depression is the primary cause of death in overdose situations. Furthermore, both substance classes can impair cognitive function, making the combination particularly hazardous.
Research consistently demonstrates that individuals who concurrently use opioids and benzo pills face a significantly increased risk of severe health emergencies. This includes higher rates of emergency department visits, hospital admissions for drug-related crises, and, tragically, death from drug overdose.
For instance, a study conducted in North Carolina revealed a stark reality: the overdose death rate among patients prescribed both opioids and benzo pills was ten times higher than those only receiving opioids. Another study focusing on U.S. veterans with opioid prescriptions found a direct link between receiving a benzo pill prescription and an elevated, dose-dependent risk of fatal drug overdose.
Recognizing this serious threat, the CDC’s Clinical Practice Guideline for Prescribing Opioids for Pain strongly advises clinicians to exercise extreme caution when considering prescribing benzo pills alongside opioids. A careful evaluation of benefits versus risks is crucial in such cases. Both prescription opioids and benzodiazepines now carry boxed warnings from the U.S. Food and Drug Administration (FDA). These boxed warnings, the FDA’s most stringent safety alerts, explicitly highlight the potential and amplified dangers of using these medications in combination.
For anyone prescribed medication, it is paramount to disclose all other substances and medications being used. Open communication with healthcare providers about potential risks and interactions is essential for safely managing medications and avoiding the potentially deadly consequences of combining drugs like opioids and benzo pills.
References
[1] National Institute on Drug Abuse. (2023, January 19). Benzodiazepines and Opioids. National Institutes of Health. https://nida.nih.gov/drug-topics/opioids/benzodiazepines-opioids
[2] Centers for Disease Control and Prevention. (2023, March 24). Polysubstance Use. National Center for Injury Prevention and Control, Division of Overdose Prevention. https://www.cdc.gov/stop-overdose/caring/polysubstance-use.html
[3] National Institute on Drug Abuse. (2023, August 9). Overdose Deaths Involving Opioids. National Institutes of Health. https://nida.nih.gov/drug-topics/opioids/opioid-overdose-crisis
[4] Park, T. W., Saitz, R., Ganoczy, D., Ilgen, M. A., & Bohnert, A. S. B. (2015). Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: case-cohort study. BMJ, 350, h2695.
[5] Gomes, T., Juurlink, D. N., Dhalla, I. A., Cornish, S., Holloway, C., & Mamdani, M. M. (2011). Co-prescribing of opioid analgesics and benzodiazepines and risk of adverse outcomes. CMAJ : Canadian Medical Association journal, 183(18), E1151–E1158.
[6] Dasgupta, N., Funk, M. J., Proescholdbell, S., Hirsch, A., & Ribisl, K. M. (2011). Cohort study of the impact of opioid analgesic and benzodiazepine co-prescribing on mortality. Pharmacoepidemiology and drug safety, 20(5), 424–431.
[7] Bohnert, A. S., Ilgen, M. A., Galea, S., McCarthy, J. F., Valenstein, M., & Blow, F. C. (2011). Benzodiazepine use and risk of mortality among patients receiving opioid analgesics. JAMA, 305(8), 798–806.
[8] Dowell, D., Ragan, K. R., Jones, C. M., Baldwin, G. T., & Chou, R. (2022). CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022. MMWR. Recommendations and Reports, 71(3), 1–95.