Benzodiazepine (BZD) abuse has escalated to alarming levels, leading to serious health consequences, particularly when combined with other central nervous system depressants. The co-abuse of BZDs with opioids and alcohol is especially prevalent, contributing to a surge in emergency department visits and fatalities in recent years. While benzodiazepines alone are rarely the sole cause of death, the broader issue of prescription drug abuse, including BZDs, demands increased attention. Despite their potential for misuse, BZDs are generally considered to have a low abuse potential in the general population. However, certain individuals, particularly those with a history of substance use disorders, are at a heightened risk. Education, preventative measures, and early identification are crucial strategies to mitigate Benzo Drugs Abuse effectively.
Introduction to Benzodiazepines and Abuse
Benzodiazepines were first introduced to the US market in 1960, with chlordiazepoxide leading the way as the first approved drug in this class for clinical use.1 BZDs quickly gained favor due to their perceived safer profile compared to older medications like barbiturates, primarily due to a reduced risk of respiratory depression.1,2
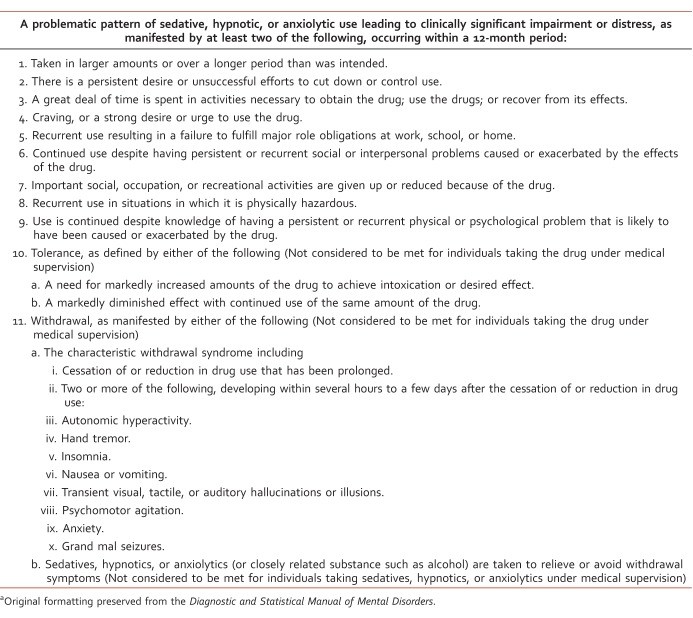
Almost two decades after their introduction, the mechanism of action of benzodiazepines began to be understood.1 BZDs enhance the activity of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter, by facilitating its binding to the GABAA receptor. This interaction ultimately increases chloride ion flow through ligand-gated chloride channels, resulting in a calming effect.3 Concurrently with the discovery of their mechanism, clinicians started to recognize the potential for benzo drugs abuse and dependence.1 The diagnostic criteria for sedative, hypnotic, or anxiolytic use disorder are detailed in Table 1, as outlined in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition.4
TABLE 1: Diagnostic criteria for sedative, hypnotic, or anxiolytic use disorder (DSM-5).
Despite the long-standing awareness of their addictive potential, understanding how to identify at-risk individuals and effectively treat benzo drugs abuse remains a challenge. While prescription drug abuse has gained increased attention, research has primarily focused on prescription opioid abuse. Benzodiazepines, despite the risks and the availability of safer alternatives, remain among the most frequently prescribed medications.5
Prevalence of Benzodiazepine Misuse
In 2008, approximately 75 million prescriptions for benzodiazepines were written in the United States alone.5 The general population prevalence of BZD use ranges from 4% to 5%.5,6 Benzodiazepine usage increases with age, and women are prescribed BZDs roughly twice as often as men.5,7 Notably, individuals already prescribed opioids are significantly more likely to also receive a BZD prescription.7,8
While most individuals use BZDs as prescribed, a small percentage, less than 2%, escalate to high doses, and an even smaller fraction meet the criteria for benzo drugs abuse or dependence.9,10 In the broader population, benzodiazepines exhibit a relatively low potential for abuse.11 However, a specific subgroup of individuals faces a higher risk of benzo drugs abuse, particularly those with a personal or family history of substance use disorders.12 Benzodiazepine abuse can manifest in two primary patterns: deliberate or recreational abuse aimed at achieving a “high,” and unintentional abuse, which starts with legitimate use but progresses to inappropriate use over time.13
Misuse and abuse of BZDs are increasingly becoming a significant public health concern. An estimated 2.3% to 18% of Americans have misused sedatives or tranquilizers, including benzodiazepines, for nonmedical purposes at some point in their lives.14–16 Nearly 10% of these individuals met the diagnostic criteria for abuse or dependence.14 In 2010, there were approximately 186,000 new cases of benzo drugs abuse.17 Emergency departments (EDs) have reported a dramatic 139% increase in BZD-related visits.18 Advanced age and the presence of other drugs were associated with more severe outcomes, including death.19 Furthermore, admissions to treatment programs for benzo drugs abuse nearly tripled between 1998 and 2008, while admissions for all substance abuse treatment programs increased by only 11% during the same period.20
Risk Factors for Benzo Drugs Abuse
The risk factors and demographics associated with benzo drugs abuse present some notable differences compared to other substance abuse populations. Firstly, non-Hispanic white individuals are disproportionately represented. The role of gender is less clear, as studies show varying predominant genders among BZD abuse populations.15,16,20–22 Young adults aged 18 to 35 years constitute the largest segment of benzo abusers.20,21 A strong correlation exists between BZD use, misuse, and abuse, and comorbid psychiatric disorders, as well as personal or family histories of substance use disorders.12,15,23,24 Comorbid psychiatric disorders are more prevalent in benzo abusers than in other substance abuse populations.20,21 Approximately 40% of individuals struggling with benzo drugs abuse also report a co-occurring psychiatric disorder. This highlights the critical need for clinicians to address both the underlying mental health condition and the substance abuse simultaneously.20 Individuals with a history of alcohol abuse or dependence, and those with antisocial personality disorder, appear to be at a particularly elevated risk of benzo drugs abuse compared to those without these conditions, or those with alcohol abuse alone.22
The Dangers of Polysubstance Abuse with Benzos
Benzo drugs abuse most often occurs in combination with other substances. For the majority, BZDs are secondary drugs of abuse, with a smaller proportion reporting BZDs as their primary drug of abuse.20 The most common primary drugs of abuse among benzo abusers are opioids (54.2%) and alcohol (24.7%).21 It’s estimated that about 1 in 5 individuals abusing alcohol also misuse benzodiazepines.22,25 BZDs are often used to amplify the euphoric effects of other drugs, to reduce unwanted side effects like insomnia from stimulants, and to manage withdrawal symptoms.2,26,27 Individuals who abuse BZDs alongside other drugs tend to consume significantly higher doses of benzodiazepines than those who abuse only BZDs.28
In 2010, BZDs were implicated in 408,021 emergency department visits, representing one-third of all ED visits related to pharmaceutical misuse and abuse.18 Specifically, ED visits due to the nonmedical use of BZDs in combination with opioids increased dramatically, from 11 per 100,000 in 2004 to 34.2 per 100,000 in 2011. The involvement of BZDs in opioid-related deaths also saw a significant rise, from 18% in 2004 to 31% in 2011. Opioids and BZDs are the two most frequent classes of prescription drugs involved in overdose fatalities.29 Overall death rates related to prescription drugs have surged in recent years.30 Individuals prescribed both a BZD and an opioid had an almost 15-fold increased risk of drug-related death compared to individuals not prescribed either medication.31 Admissions to treatment programs for combined opioid and benzo drugs abuse witnessed a staggering 570% increase from 2000 to 2010.21
Opioids are known to cause respiratory depression, and this effect is compounded when combined with BZDs or alcohol. The interaction between opioids and BZDs is complex, involving the interplay of excitatory and inhibitory neurotransmitter systems in respiration control. While BZDs alone are weak respiratory depressants and rarely cause death,2,12,33,34 their combination with opioids can result in potent respiratory depression.32 Opioids reduce the body’s sensitivity to changes in oxygen and carbon dioxide levels and decrease tidal volume and respiratory frequency.3,32 Tolerance to opioid-induced respiratory depression develops slowly and incompletely compared to analgesic tolerance.32
Patients undergoing opioid replacement therapy with methadone or buprenorphine are particularly vulnerable to benzo drugs misuse and abuse.35–37 Reasons for this increased risk include high levels of psychological distress, recreational use, sleep problems, withdrawal symptom management, mitigation of stimulant side effects like insomnia, and a misperception that BZDs are not dangerous.35,36 Studies show lifetime BZD abuse prevalence as high as 66.3% and current abuse at 50.8% in methadone maintenance patients.36 Alarmingly, over half of BZD users in methadone programs started using benzodiazepines after beginning methadone treatment.38 The combination of BZDs and methadone is associated with a 60% increase in opioid-related deaths.39 While buprenorphine has an advantage over methadone due to its ceiling effect on respiratory depression, this protective effect diminishes when combined with BZDs.40 Among buprenorphine-experienced individuals, 67% reported concurrent BZD use, with about one-third obtaining BZDs from multiple or illicit sources.37
Alcohol is a factor in 1 in 4 ED visits related to benzo drugs abuse and 1 in 5 BZD-related deaths.18 Both alcohol and BZDs interact with the GABAA receptor, leading to synergistic central nervous system depression. This pharmacodynamic interaction results in additive effects, meaning lower concentrations of each substance can lead to fatal outcomes.41 BZD-related ED visits combined with alcohol are most common in individuals aged 45 to 54, while deaths are more frequent in those 60 and older.42 Despite alcohol’s significant role in various health issues, recent data suggests only 1 in 6 adults in the US have ever discussed their alcohol use with a healthcare professional.43 It’s crucial for prescribers and pharmacists to educate patients about the risks of combining alcohol and BZDs and for healthcare professionals to intervene and refer patients when problematic alcohol consumption is suspected or identified.
Abuse Liability of Different Benzodiazepines
Systematic studies comparing the abuse potential within the benzodiazepine class are lacking. However, pharmacokinetic properties are believed to play a role in abuse liability. Lipophilicity, a chemical property affecting the speed of drug entry into the brain, influences the onset of action.44 BZDs with higher lipophilicity and shorter half-lives appear to have a greater potential for abuse.11,13 Table 2 presents the chemical properties of common benzodiazepines.44 Evidence from laboratory studies, medical professional experience, user accounts, and epidemiological data suggests diazepam has a particularly high abuse liability.45 Diazepam, alprazolam, and lorazepam received the highest subjective ratings for the “high” they produce among drug abusers, compared to oxazepam, clorazepate, and chlordiazepoxide, which are considered to have lower abuse potential.2,11,45,46 In blinded studies, recreational drug users rated diazepam as more desirable than equipotent doses of alprazolam and lorazepam.47 Despite this, alprazolam and clonazepam are the BZDs most frequently linked to abuse-related ED visits, with alprazolam involvement being more than double that of clonazepam.48 Alprazolam is also the most prescribed BZD in the US, with over 44 million prescriptions dispensed in 2009, almost twice the number of clonazepam prescriptions, the second most prescribed BZD.49 Ease of access likely contributes to alprazolam’s high abuse rates.49 While pharmacokinetics and user preferences are important factors in abuse potential, prescribing patterns and drug availability likely play an equally significant role in benzo drugs abuse.50
TABLE 2: Chemical properties of common benzodiazepines.
Implications for Healthcare Professionals in Combating Benzo Drugs Abuse
Prescription drug diversion originates from various sources, both healthcare-related and non-healthcare-related. The most frequently reported healthcare source of BZD diversion is a regular prescriber, followed by “script doctors,” “doctor shopping,” and pharmacy diversion.51 Recommendations for identifying high-risk individuals and reducing benzo drugs abuse include: obtaining thorough personal and family substance use histories, urine drug screening, frequent monitoring for signs of abuse, reassessing the risks and benefits of ongoing therapy, prescribing limited “as-needed” doses to minimize physiological dependence, and differentiating between physical dependence and addiction.12
“Pharmacy shoppers,” defined as individuals receiving the same BZD prescription at two pharmacies within 7 days, are at a 5.2 times greater risk of escalating to high BZD doses compared to other long-term BZD users.9 “Doctor shoppers,” or individuals visiting 4 or more clinicians in a 6-month period, are more likely to be female and have twice the risk of drug-related death compared to non-shoppers. “Pharmacy shoppers,” defined as individuals filling controlled substance prescriptions at 4 or more pharmacies within 6 months, have a 3 times higher risk compared to non-shoppers.31,32 Prescription drug monitoring programs are valuable tools in identifying prescription drug abuse patterns.
Over 90% of unintentional pharmaceutical overdose fatalities show at least one indicator of substance abuse, including known history of substance abuse, drug diversion, nonmedical routes of administration, multiple prescribers of controlled substances, alcohol or illicit drug use, previous overdose, and current opioid replacement therapy.33 Prescribers and pharmacists must be aware of these risks, utilize prescription drug monitoring programs, accurately identify drug abusers, and implement appropriate risk mitigation strategies. Additional strategies to reduce abuse include limiting dose, quantity, and refills on each prescription.52 Diversion is most prevalent among young adults, who often obtain drugs from peers or family members.8,33,52
Past initiatives to restrict benzodiazepines, like the triplicate prescription program in New York in 1989, aimed to reduce prescribing by requiring multiple copies of prescriptions and limiting supply.53 While these measures did reduce overall benzodiazepine prescribing, they also had unintended negative consequences, disproportionately affecting low-income and minority populations and hindering access to appropriate medical care.53–56 Healthcare providers and lawmakers must exercise caution when implementing strategies to combat prescription drug abuse to avoid negatively impacting appropriate patient care.
Some clinicians argue that the medical community may have overreacted to the risks of benzo drugs abuse, potentially leading to underprescribing of a valuable class of medications. They advocate for responsible and continued benzodiazepine prescribing when medically necessary.57 While benzodiazepines do carry abuse potential, especially in substance abuse populations, it’s essential to balance these risks with the therapeutic benefits. Prescribers must also consider the risks of untreated conditions, as poorly managed anxiety or insomnia can increase the risk of alcohol relapse.58 Evidence-based pharmacotherapy and non-addictive alternatives should be prioritized, but BZDs may still be indicated for certain high-risk patients. In such cases, thorough patient education on the risks of combining BZDs with alcohol or other substances, discussion about diversion risks, prescribing BZDs with lower abuse potential, and careful monitoring for adverse effects and misuse are crucial.
Conclusion: Addressing the Epidemic of Benzo Drugs Abuse
Prescription drug abuse has reached epidemic proportions, and current efforts to curb associated morbidity and mortality have not been effective, with rates continuing to rise. Further research is essential to better understand the risk factors for benzo drugs abuse. Despite the risks of abuse and diversion, BZDs remain a valuable and effective class of medications with a continued role in therapy. Lawmakers and healthcare professionals face the challenge of reducing abuse while ensuring accessibility for patients who genuinely need these medications. Emphasis should be placed on reducing inappropriate prescribing rather than restricting all prescribing. Education is paramount. Healthcare professionals must stay informed about abuse patterns and diversion trends. It is imperative for prescribers and pharmacists to educate patients not only about personal risks but also the risks of medication sharing to others. Identifying benzo drugs abuse risk factors before prescribing, utilizing safer alternatives when possible, and implementing appropriate interventions to address ongoing abuse are critical steps. Expanding substance abuse treatment programs and increasing funding for these programs will be a vital component in tackling this growing public health crisis.
Footnotes
Disclosures: This material is the result of work supported with resources and the use of facilities at the Fargo Veterans Affairs Health Care System. The contents do not represent the views of the Department of Veterans Affairs or the US government.